Actions in the Region
MSF’s operational footprint in the region.
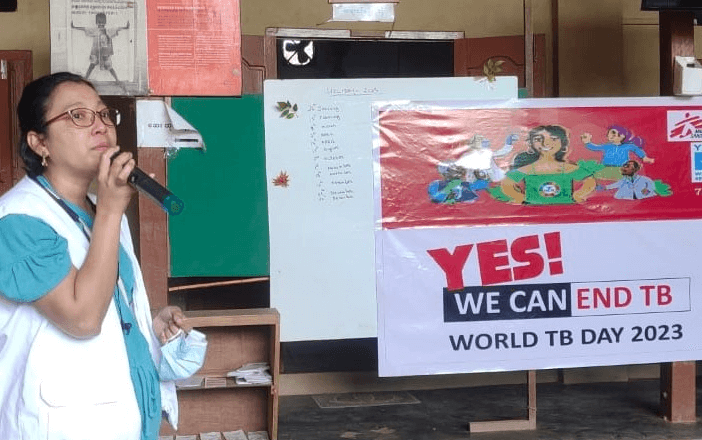
MSF has projects in the region -- in Hong Kong, Philippines, Indonesia, Malaysia, Cambodia, Myanmar, Thailand -- during the past decades. Some projects, such as in mainland China, were handed over in 2014. These projects varied depending on the medical and humanitarian needs of the people throughout the years. Some projects were in response to the aftermath of major natural disasters; addressing Hepatitis C, HIV, and Tuberculosis; on sexual reproductive healthcare, and others.
Médecins Sans Frontières (MSF) is currently running a healthcare project to support local homeless people in Sham Shui Po and Yau Tsim Mong districts.
Find out more: “Hong Kong: MSF launches healthcare project to support local homeless community”
MSF started working in Hong Kong in 1988 during the height of an influx of Vietnamese boat people. For 10 years we ran outpatient clinics with medical referral services, offered antenatal care and extended programmes of immunisation, and launched psychological support programmes. We gave health education, which focused on the prevention of HIV/AIDS and other sexually transmitted diseases and conducted a harm reduction needle exchange programme for heroin addicts.
During the SARS outbreak in Hong Kong in 2003, MSF set up an information, education and communication programme at the peak of the epidemic and mobilised more than 100 medical and nursing students and local medical doctors to bring SARS prevention messages to public housing estates and ethnic minority communities.
MSF's responded to the COVID-19 outbreak in the city when an emergency team was mobilised to respond to the outbreak in January 2020. We focused on groups who are less likely to have access to important medical information, such as street cleaners, foreign domestic helpers, visually impaired people, the homeless, refugees and asylum seekers; and those who are more vulnerable to developing severe disease if they are infected such as the elderly.
The team collaborated with local NGOs to offer a people-centred vaccination programme, which included free medical consultations and inoculation for vulnerable groups, and we also provided telehealth support. A mental health website was created for the general public, offering tips and tools to help cope with these stresses and worries due to prolonged exposure to uncertainty.